Learn what soy allergy is, symptoms of soy allergy, soy allergy trends, and the many hidden sources of soy that people with soy allergies need to avoid.
Soy allergy is one of the top 8 food allergies in the United States. It is largely a food allergy that affects young children, mostly infants and toddlers under the age of 3. Although many children with soy allergies outgrow their allergy when they get older, some soy allergies persist into adulthood and become lifelong. Soy allergies can be especially challenging, because soy is hidden in so many foods. They also have the potential to cause life-threatening anaphylaxis.
Here’s what parents need to know about soy allergies.
What is a Soy Allergy?
Soy is a member of the legume family (it’s in the same family as peanuts, peas, and other beans). A soy allergy is an allergy to the soybean plant, as well as to foods like soybean oil and soy milk that are made from the soybean plant.
Our immune systems normally defend and protect us from viruses, bacteria, and other harmful invaders. But when someone has a soy allergy, their immune system mistakenly treats soy proteins as harmful invaders, and over-defends the body against these soy proteins. This causes an allergic reaction whenever the person eats soy.
Even though soybeans are in the same family as peanuts (the legume family), having a soy allergy doesn’t increase someone’s risk of developing a peanut allergy.
Learn more about this top allergen from Food Allergy Research & Education (FARE):
Categories of Soy Allergies
There are two main categories of soy allergies: IgE-mediated and non-IgE-mediated soy allergies.
When someone has an IgE-mediated soy allergy, their immune system makes special allergy antibodies called IgE antibodies to soy proteins to help fight them off. These IgE antibodies trigger symptoms of an allergic reaction whenever the person eats a food containing soy, within seconds to hours after they eat the soy product.
Non-IgE-mediated soy allergies also involve the immune system, but they don’t involve IgE antibodies. The mechanisms behind these allergies aren’t yet well understood. This type of soy allergies causes GI symptoms hours to days after the person eats soy, so these allergies are sometimes called “delayed-type soy allergies.”
Some types of non-IgE-mediated soy allergies include food-protein-induced enterocolitis syndrome (FPIES), Food protein-induced allergic proctocolitis (FPIAP or allergic proctocolitis), and eosinophilic esophagitis (EoE). For more on these types of non-IgE-mediated food allergies, please read this article.
Symptoms of Soy Allergies
Symptoms of an IgE-mediated soy allergy can include:
- Hives (red raised bumps)
- Vomiting
- Skin redness
- Itching
- Itchy, watery eyes
- Swelling of the face, lips, eyes, tongue, or throat
- Runny nose
- Congestion
- Wheezing
- Difficulty swallowing
- Difficulty breathing
- Nausea
- Diarrhea
- Abdominal pain
- Dizziness
- Fainting
Symptoms of an IgE-mediated soy allergy usually develop seconds to minutes after eating a soy product, and almost always within 2 hours.
Symptoms of a non-IgE-mediated soy allergy can include:
- Vomiting
- Diarrhea
- Stomach pain
- Abdominal pain
- Abnormal stools
- Decreased appetite/refusal to eat
- Difficulty gaining weight
- Reflux-like symptoms
- Irritability
- Other GI symptoms
Symptoms of a non-IgE-mediated soy allergy usually emerge hours to days after eating a soy product.
Soy allergic reactions can range from mild to severe. When the symptoms of a soy allergic reaction are severe, and involve more than one organ system, the reaction is classified as anaphylaxis. And anaphylaxis can be life-threatening.
(IgE-mediated soy allergies are much more likely to cause anaphylaxis than non-IgE-mediated soy allergies.)
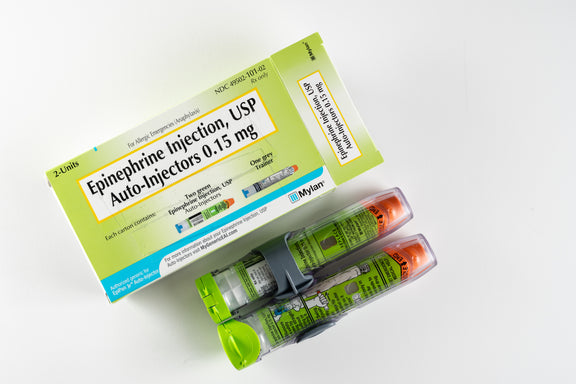
Swelling of the face, tongue or throat, wheezing, breathing difficulty, and significant cardiovascular symptoms may be signs of an anaphylactic reaction. If your child shows signs of anaphylaxis, give epinephrine (use an Epi-Pen) immediately, and call 911.
Soy Allergy Testing
IgE-mediated soy allergies can be diagnosed through:
- A skin prick test (where your child's forearm is pricked with a needle containing soy protein, then monitored to see if an allergic reaction develops around the area where their skin was pricked)
- A blood test (where your child's blood is checked for IgE antibodies that respond to soy proteins)
- An oral food challenge (where your child eats small amounts of soy under an allergist’s supervision, to see if they develop an allergic reaction. This is the most accurate way to diagnose a soy allergy.)
These tests won’t work to diagnose a non-IgE-mediated soy allergy, though, because these tests rely on the presence of IgE antibodies or an immediate allergic reaction to soy. To determine whether your child may have this delayed type of allergy, you’ll need to remove soy from their diet for several days and see if symptoms improve, in consultation with your doctor. Then, add soy back into your child's diet and see if the symptoms reappear.
If baby’s symptoms seem tied to soy, they may have a delayed type of soy allergy. But they may have a soy intolerance instead, which is different from a soy allergy.
Soy Allergy Trends
Soy allergy is one of the top 8 food allergens in the United States.
Soy allergy affects 0.4% of children, mostly infants and toddlers under the age of 3. It affects around 0.3% of the general population (children and adults).
Most children with soy allergies eventually outgrow the allergy. One study found that around 25% of children outgrow their soy allergy by age 4, around 45% outgrow their soy allergy by age 6, and nearly 70% outgrow it by age 10.
Another study reported that “the peak prevalence of soy allergy was 1.5% at age 1 year, [but] after age 1 year, prevalence rates steadily decreased to a low of 0.2% at age 14 to 17 years.” This also shows an outgrowing of soy allergy.
However, some people never outgrow their soy allergies, and end up with lifelong soy allergies.
Since soy is one of the top 8 allergens, U.S. federal law requires all packaged food products that contain soy to state that they contain soy on the label, in clear language.
Managing A Soy Allergy
People with soy allergies need to strictly avoid all products containing soy, because eating any amount of soy could potentially trigger an allergic reaction.
This includes avoiding:
- Soy milk, soy cheese, soy yogurt and soy ice cream
- Soybean oils, including cold-pressed, extruded, and expelled soybean oil.
- Most people with soy allergies can safely eat highly refined soybean oil, but speak with your allergist to make sure this is okay for your child to eat.
- Highly refined soybean oil is not required to be labeled as a soy allergen. Manufacturers don’t need to label their product “contains soy” if their product contains this ingredient. So, if your child needs to avoid highly refined soybean oil, you’ll need to read labels even more carefully.
- Soy sauce
- Soy nuts and soy “nut butter”
- Soy protein (concentrate soy protein, hydrolyzed soy protein, isolate soy protein)
- Soy albumin
- Soy flour
- Soy fiber
- Soy grits
- Soybean curd
- Soybean granules
- Soy lecithin
- Some people with soy allergies can safely eat soy lecithin, but speak with your allergist, because this varies from person to person.
- Any other ingredient containing the word “soy” or “soybean”
Even though soy products must be clearly labeled as food ingredients under federal law, avoiding soy can still be complicated. This is because so many products contain hidden soy. Always read all food labels carefully to keep your child safe!
Sometimes, these products may contain hidden soy:
- Candies
- Chocolate bars
- Cereals
- Crackers
- Bread rolls and other baked goods
- Chicken nuggets
- Processed meats
- Plant-based “ alternative meats” (meant as vegan substitutes for meat products, like burgers and chicken; many are soy-based)
- Baby formulas (talk to your doctor about switching to an alternative without soy)
- Broths
- Margarine
- Canned meat and fish
- Low fat peanut butter
- Granola bars/nutrition bars
- Sauces
- Products with “natural flavors” (yes, the flavoring may include soy!)
Soy products also have many different names, so be on the lookout for these hidden soy types as well:
- Edamame (another name for soybeans)
- Miso (fermented soybean paste used as seasoning)
- Soya, or any product with soya in its name (another way to write “soy”)
- Shoyu (Japanese-style soy sauce)
- Tamari (another type of Japanese soy sauce)
- Teriyaki (sauce)
- Worcestershire sauce
- Kinako (soy flour)
- Nimame (simmered soybeans)
- Okara (soy pulp)
- Tempeh (cake-like fermented soybeans, somewhat like tofu)
- Tofu (blocks of condensed soy milk/soybean curd)
- Textured vegetable protein (soy-based alternative to ground meat)
Asian restaurants, including Chinese, Indian, Japanese, Indonesian, Thai and Vietnamese restaurants, can also be particularly dangerous for people with soy allergies. This is because so many foods in these restaurants contain soy---soy is a staple food in these cuisines.
Even if you order a food that you’re sure doesn’t contain soy, there’s still a high risk of cross-contamination. This is the accidental mixing of a food with soy into a food without soy.
No matter what type of restaurant (or any location where food is served) you visit, though, you’ll need to alert the person preparing food that your child is allergic to soy. With so many foods containing soy, any environment with food could pose a risk of cross-contamination.
At stores, also look out for products that say "may contain soy" or "manufactured on equipment that also processes soy." This is a sign that there was likely cross-contamination in the plant where the product was produced. So, there could accidentally be traces of soy in these products.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.

