Learn what milk allergy is, the difference between milk allergy and lactose intolerance, and tips for milk allergy management, treatment, and early milk introduction.
Milk is your baby’s top source of calcium for bone health. Calcium is more easily absorbed by the body when taken from milk than from vegetables. Despite being the first food that your baby will eat, it is also the most common food allergy among children.
What Is Milk Allergy?
With milk allergy, your child’s immune system mistakenly treats milk as a harmful invader. The body treats it much like a virus or bacteria. When the immune system detects proteins from milk, it produces allergy antibodies to ward them off. These antibodies then trigger a reaction each time you ingest milk.
Milk allergy may be confirmed through a skin-prick test or a blood test to check for immunoglobulin E (IgE) antibodies, which become present when you are exposed to allergens.
Common Milk Allergy Reactions
These are some of the most common reactions triggered by milk allergy:
Skin: Hives, rash and itching
Gastrointestinal: nausea, gas, reflux, vomiting, diarrhea
Mouth: swelling and/or itching of lips, tongue or palate
Respiratory: runny nose, sneezing, wheezing, nasal congestion
Eyes: redness, itching, hives
Parents often confuse milk allergy with lactose intolerance because their symptoms can be similar. The two, however, are not related.
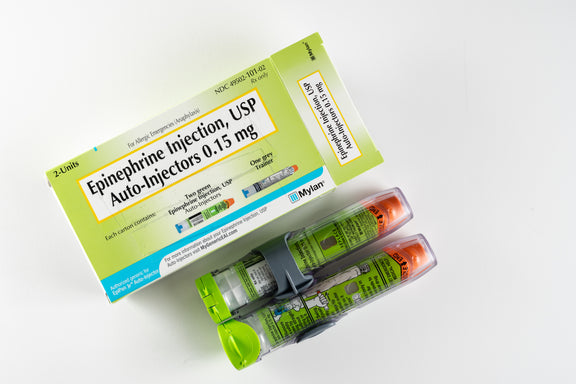
Sometimes, the allergic reaction can be severe. When it involves more than one organ system, it can signal an anaphylactic reaction. Anaphylaxis requires emergency care and is usually treated with one to two doses of epinephrine.
Can Milk Allergy Be Outgrown?
The short answer is yes, it is possible to outgrow milk allergy. It was previously thought that milk allergy will be outgrown by the time a child turns 3. However, recent studies show that only less than 20% of children with milk allergy had outgrown it by the time they turn 4. ACAAI says around 80% of these children will outgrow their milk allergy before the age of 16.
What is Lactose Intolerance?
Lactose intolerance is a type of food intolerance. The main difference between food allergy and food intolerance is the involvement of the immune system. With milk intolerance, the body doesn’t treat milk as an invader. What happens here is the body can’t digest lactose or the sugar in milk because of lactase deficiency. Lactase is an enzyme produced by the small intestine.
Lactose can’t be digested when lactase is not sufficient. This is what causes the digestive symptoms.
Common Lactose Intolerance Symptoms
- Diarrhea
- Bloating
- Abdominal cramps
- Gassiness or colic
- Nausea
These are often mistaken for milk allergy, but unlike milk allergy, lactose intolerance doesn’t cause other symptoms that are associated with allergy (like hives, itching, or anaphylactic shock).
Lactose intolerance is also more common in adults. MedlinePlus says about 30 million Americans develop lactose intolerance by the age of 20. In North America, the rate of lactose intolerance is present in 79% of Native Americans, 75% of blacks, 51% of Hispanics, and 21% of Caucasians.
In some cases, children may have lactose intolerance if they were born premature or if they have a genetic defect that makes them unable to produce the lactase enzyme. Most people are born with the ability to digest lactose. It is also found in breastmilk.
Lactose intolerance can also be caused by a viral stomach bug or other illnesses that cause inflammation in the gut.
Lactose is found in all types of cow’s milk, goat’s milk, cheese, yogurt, ice cream, and butter. Foods that use dairy products as an ingredient may contain lactose, too.
To test your child for lactose intolerance, your healthcare provider may request for the following tests: lactose tolerance test, hydrogen breath test, and stool acidity test.
Milk Allergy Trends
Milk is the most common food allergy in infants and young children. This usually manifests in a child’s first year of life. Around 2 to 3 percent of children under 3 years of age are allergic to cow’s milk or a milk protein from animal sources, according to the American College of Allergy, Asthma & Immunology(ACAAI). Although most children outgrow milk allergy or become more tolerant to milk, it still is one of the most common causes of allergic reactions in school.
The Impact of Food Allergy
Children with milk allergies may experience social exclusion and activity avoidance. Imagine going to parties where milk and food with dairy products like ice cream and cake are served. It can be difficult for the child. It can also be difficult for the parent to monitor their child’s food intake when they are not around. A 2014 study also reveals that 1 in 3 children with allergies has experienced bullying.
Management and Treatment
At present, there is no cure for milk allergy and any other type of food allergy. To maintain safety, allergists recommend strictly avoiding allergens and nutritional counseling. This includes learning to read food labels, identifying hidden ingredients, avoiding cross-contact, and recognizing early signs of anaphylaxis and when to administer epinephrine.
Immunotherapy is offered as a food desensitization treatment, which includes oral, sublingual, and epicutaneous immunotherapy. These all involve introducing small doses of allergenic food to develop tolerance. This form of treatment has not yet been proven to work.
Mild allergic symptoms like hives, runny nose, itchy mouth, and upset stomach can be treated with antihistamines prescribed by your healthcare provider.
Severe symptoms manifesting as two or more symptoms from different body areas, difficulty breathing, or significant swelling require epinephrine injection immediately. Emergency care must be sought as soon as possible even after administering epinephrine. This is because more serious symptoms might show up later on.
Introducing Cow's Milk Early
Current research shows that early introduction of allergenic foods like milk, eggs, and nuts as early as 4 months of age is recommended. The key is sustained allergen introduction where you frequently feed your baby allergenic foods multiple times a week for a long period of time. It is recommended to introduce one allergenic food at a time every few days.
If you feel that 4 months of age may be too early to introduce solid foods, you can check your baby’s readiness based on these cues from the American Academy of Pediatrics:
- Sitting up with minimal support
- Achieving strong head control, i.e. can hold head up for an extended period of time
- Showing interest in food, i.e. trying to grab food off your plate
- Turning head away from the bottle or breast when not hungry
Get more tips for introducing solid foods to your baby.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.

