When your baby has rough, scaly, or itchy rash, you may wonder if it’s eczema. Learn symptoms of eczema, where it usually appears, and how it's diagnosed.
When your baby has rough, scaly, or itchy rash, you may wonder if it’s eczema. Eczema’s symptoms and appearance may change at every stage of your baby’s life, so it is important to consult your child’s doctor if the rash doesn’t go away. Your baby’s doctor will be able to confirm whether your child’s skin symptoms are indeed signs of eczema by examining the skin, checking your baby’s medical history, other symptoms and risk factors.
What is Eczema?
The National Eczema Association defines eczema as “a group of conditions that cause the skin to become red, itchy, and inflamed.” It is common in children and may appear as early as the first six months of your baby’s life. Eczema has several types, with atopic dermatitis as the most common type. Eczema is not contagious.
What Are the Signs and Symptoms of Eczema?
- Patches of red or dry skin.
- Rough and itchy skin.
- Crusty scales and bumps that may leak fluid.
These symptoms may not be permanent and may flare-up when exposed to certain triggers, like food or environmental allergies. In addition to allergens, dry skin, heat, infection, and irritants may trigger eczema. This condition may be present in children who have asthma or allergies.
Where Does Eczema First Appear?
For infants, the symptoms first appear as a rash on their cheeks, forehead, or scalp. You may also see them on the joints of your baby’s arms and legs. The diaper area is usually spared because it is moist.
Cradle cap or seborrheic dermatitis commonly affects babies. In young children, you may see eczema on the cheeks, knees, head, and elbows. Babies may scratch these areas and give you a clue whether they have eczema. If it gets infected, you may notice crusting or formation of pus bumps on the skin.
How Is Eczema Diagnosed?
There is no single test that can diagnose eczema. The rash will get examined by the doctor and ask about your child’s health and family history. Some factors that commonly trigger eczema are heat, dry skin, dry air, infection, allergens, and irritants. Your baby’s saliva is also an eczema trigger.
Dermatologists use a SCORAD (Scoring Atopic Dermatitis) tool to evaluate the severity of your child’s eczema. It may be classified as mild, moderate or severe. They take into account the areas or sites affected, the intensity of the symptoms, and itch or sleeplessness. Most eczema cases are only mild to moderate. Eczema is usually outgrown when the child starts school or by 5 to 6 years old.
If your baby has eczema, your doctor may prescribe moisturizers, anti-inflammatory medicines, and hydrocortisone creams or ointments. Antibiotics may also be prescribed if there is a bacterial infection or when there are blisters with pus.
If you think that your child has eczema symptoms, it is best to see an allergist or a dermatologist who can confirm whether your child has eczema and recommend the right treatment plan.
The Link Between Allergies and Eczema
There is a strong link between allergies and eczema in babies. Up to 67% of babies with severe eczema will develop a food allergy, so food allergen introduction is vital. The AAP, NIH, and FDA all agree that feeding your baby allergens like peanut and egg should be done starting as early as 4 months.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
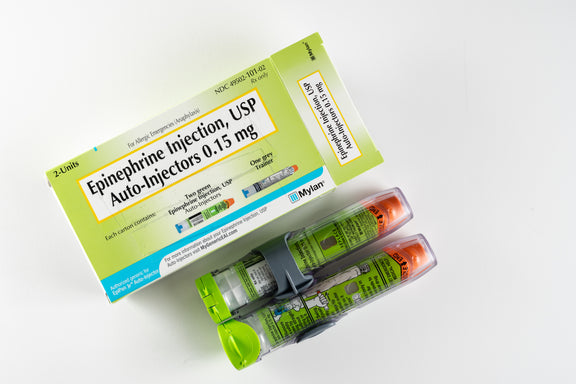
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.

