What are fruit allergies, and what do the different types of fruit allergy reactions look like? How can you manage your child’s fruit allergies? We answer all these questions and more in this fruit allergy guide.
Although fruit allergies aren't part of the top 9 food allergens, they're more common than you think. Daniel Tiger from the beloved children's series Daniel Tiger's Neighborhood even has a fruit allergy – he is allergic to peaches.
Today, we'll go over what fruit allergies are, what fruit allergy reactions look like, and how to manage your child's fruit allergies.
What are fruit allergies?
Fruit allergies always involve the immune system. When someone has a fruit allergy, their immune system sees the fruit they're allergic to as a threat, and causes the body to over-react when they consume that fruit.
What are the most common fruit allergies?
Someone could develop an allergy to any fruit. But the most common fruit allergies are to:
- Apples
- Kiwi fruit
- Pears
- Members of the melon family (like watermelon, cantaloupe, and honeydew)
- Stone fruits (like peaches, plums, mangoes, and cherries)
There are many other fruits that people have commonly developed allergic reactions to as well, including:
- Bananas
- Citrus fruit (like oranges)
- Pineapples
- Strawberries
- Grapes
Oral Allergy Syndrome
Most of the time, fruit allergies are linked to oral allergy syndrome, also called pollen food allergy syndrome or PFAS. When someone has PFAS, they are allergic to both certain types of pollen and certain fruits, vegetables, or tree nuts.
Oral allergy syndrome only develops in children and adults who already have a pollen allergy – so, they have the pollen allergy before the fruit allergy. It’s extremely rare for babies and toddlers younger than 3 years old to develop PFAS, because children usually don’t develop pollen allergies until after age 3.
What happens when someone has oral allergy syndrome (PFAS)?
Here’s what happens in someone’s body when they have a PFAS allergy to fruit:
- Their immune system recognizes that the proteins in certain fruits are very similar to the structure of the pollen types they are allergic to.
- So, their immune system sees both the pollen and the similar fruit proteins as threats.
- Whenever this person eats certain raw fruits or vegetables, their immune system thinks the fruit and vegetable proteins are the same as the “problem” pollen.
- The immune system over-defends the body against the fruit proteins, and triggers symptoms of an allergic reaction to develop (This is known as cross-reactivity.)
Which fruits are similar to which pollens?
These fruits (and other foods) are similar to certain pollens, so eating them may cause symptoms if someone has PFAS and an allergy to a given pollen.
|
Pollen |
Fruits with similar proteins |
Other foods with similar proteins |
|
Grass |
Peaches, oranges, and melons |
Tomatoes and celery |
|
Birch |
Apples, peaches, pears, plums, nectarines, kiwi, apricots, cherries |
Celery, carrots, bell peppers, almonds, walnuts, hazelnuts |
|
Ragweed |
Melons and bananas |
Cucumber and zucchini, |
|
Alder |
Apples, pears, peaches, cherries |
Celery, almonds, hazelnuts |
|
Mugwort |
Apples and kiwi |
Celery, carrots, bell peppers |
Can someone with oral allergy syndrome eat cooked fruit?
Many people with oral allergy syndrome to fruits only develop allergic reactions to the raw fruits. They can often eat their "problem” fruits without any issues as long as those fruits are cooked. This is because cooking usually distorts the “problem” fruit proteins enough that the immune system no longer recognizes them.
What are the symptoms of oral allergy syndrome?
The most common symptoms of pollen food allergy syndrome include:
- Scratchy throat
- Itchy or tingly mouth
- Itchy or tingly tongue
- Congestion
- Sneezing
- Swelling of the mouth, lips, throat, or tongue
- Hives on the mouth area (sometimes)
- Itchy ears (sometimes)
Most of the time, oral allergy syndrome only causes symptoms in the mouth and on the face area. Symptoms will usually develop minutes after someone eats a “problem” food. If the “problem” food is swallowed or spit out, the symptoms will usually resolve quickly.
PFAS reactions are usually mild, and hardly ever severe. They are usually milder than traditional food allergy reactions.
Very few people have developed a severe reaction, and even fewer have developed anaphylaxis (a whole-body, life-threatening allergic reaction) from PFAS.
But there’s still a small chance that a PFAS reaction could become severe. So if your child has PFAS, avoid feeding them their “problem” foods.
Other fruit allergies
Although it isn’t as common, someone can also develop a fruit allergy that isn’t connected with pollen allergies. Sometimes, people will develop fruit allergies that trigger the symptoms of traditional IgE-mediated food allergies. People could develop this type of fruit allergy at any age. So, if your child is under the age of 3 and starts having an allergic reaction to fruit, this is likely the type of fruit allergy they have.
What happens in the body with this type of fruit allergy?
Even though this type of fruit allergy is different from PFAS, similar things happen in the immune system. When someone has this type of fruit allergy, their immune system sees typically harmless fruit proteins as harmful invaders. Their immune system over-defends the body against the fruit proteins, and triggers symptoms of an allergic reaction whenever they eat their “problem” fruit.
Managing a “traditional” fruit allergy
People with this type of fruit allergy need to avoid eating their problem fruit completely, as eating even a small amount of their problem fruit will cause them to develop an allergic reaction. Be sure to read packaged food labels carefully, to make sure foods don’t contain the fruit(s) your child is allergic to.
If someone has this type of fruit allergy, they won’t be able to eat their “problem” fruit even if it’s cooked, as there’s a chance that their immune system will still recognize the fruit proteins and trigger an allergic reaction. This type of fruit allergy is also much more likely to cause life-threatening anaphylaxis than PFAS is.
What are the symptoms of a “traditional” fruit allergy?
In babies and young children, hives (rounded raised bumps) and vomiting are the most common symptoms of this type of fruit allergy.
Other mild symptoms of this type of fruit allergy may include:
- Redness in one area of the skin
- Swelling of the face, eyes or lips
- Itchiness
- Itchy, watery eyes
- Congestion
- Sneezing
- Some stomach pain
- Some nausea
- Mild coughing
Severe symptoms of this type of fruit allergy may include:
- A food allergy rash that spreads to many areas the body
- Swelling of the tongue
- Swelling or tightness of the throat
- Repeated, significant coughing
- Wheezing/noisy breathing
- Difficulty breathing /shortness of breath
- Change in voice or cry
- Struggling to vocalize
- Difficulty swallowing
- Repeated vomiting
- Pale appearance
- Diarrhea
- Dizziness
- Fainting
- Drop in blood pressure
- Rapid heartbeat
- Loss of consciousness
- Feeling floppy (infants/young children only)
Symptoms of this type of fruit allergy reaction usually occur seconds to minutes after someone eats a fruit they’re allergic to, and almost always occur within a few hours of eating the fruit.
Since symptoms vary from reaction to reaction, there’s no way to predict the symptoms that will emerge when someone eats their “problem” food. It’s also impossible to predict whether a reaction will be mild or severe. It’s also important to remember that a reaction that starts out mild could turn severe.
If your child develops any symptoms of a “traditional” fruit allergy reaction, stop feeding them the problem fruit immediately and seek medical advice.
- In the case of a mild or moderate allergic reaction, call your pediatrician
- If the reaction is severe, seek emergency medical attention.
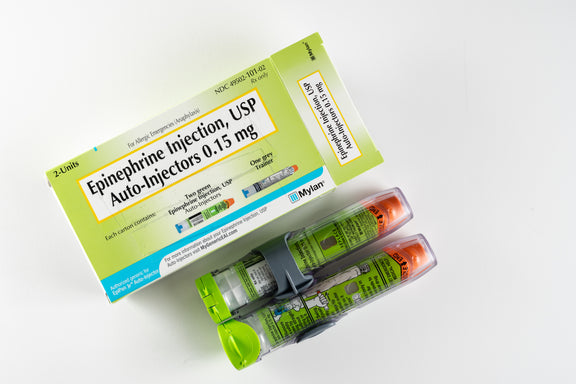
If the symptoms of a fruit allergy reaction are severe and involve more than one organ system, this is known as anaphylaxis. Anaphylaxis can be life-threatening. If your child shows signs of anaphylaxis, give epinephrine (use an Epi-Pen) immediately. Then, call 911.
-------------------------------
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease.
See the FDA Peanut Allergy Qualified Health Claim at the bottom of our homepage.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.
