We’re excited to partner with The Pump Station and Nurtury, a trusted local and national resource for breastfeeding support and Corky Harvey RN, IBCLC, MS, The Pump Station and Nurtury Founder and Lactation Consultant, to discuss common questions about breastfeeding.
What can I do if my baby doesn’t latch right away?
In order to effectively take milk, a baby must latch onto the breast and be able to sustain the attachment. The deeper the latch, the more easily the baby takes mother's milk, and the more comfortable the mother will be. Be prepared. Take a prenatal breastfeeding class with your partner, and know where help can be found once the baby arrives
If you’re having a hard time getting your baby to latch, here are some helpful tips:
- Ask for help. If still in the hospital be persistent with the staff about seeing a lactation consultant. If at home, contact a lactation professional to arrange a consultation. In this era, virtual consultations are extremely helpful.
- Do lots of time with the baby skin-to-skin.
- Try different positions. Football hold is a favorite for helping with difficult latch.
- Tip baby’s head slightly back (extended) and place the nipple lightly in the curve of the upper lip. Let the baby root (open) widely allowing the lower jaw to drop well back of the nipple base. Now tilt baby’s head forward, bringing the mouth up over the top of the breast. The lower jaw should be positioned more deeply than the upper jaw. It’s a two-point landing—lower jaw, upper jaw. (Check out the latch video on our website).
- Shaping the breast can help. Make sure to keep the fingers off to the side, out of the way, as the breast is compressed to fit more easily into the baby’s mouth.
IMPORTANT: If in spite of best efforts, the baby is still not latching, pumping the breasts 8-plus times/day is an absolute MUST. Milk supply is a Take/ Make situation; removing milk drives the supply. It will be small amounts at first but stick with it and the milk will come. All pumps are not the same; a good quality pump is very important.
I strongly believe that with a good milk supply, a bit of help, a little time and patience, that almost every breastfeeding problem can be resolved.
When is the best time to introduce a bottle?
Ideally introduce the bottle when the baby is between 2 and 4 weeks of age, and use a slow flow nipple. Continue to offer a bottle at least 3 times a week and as much as once a day. Waiting too long may result in the baby refusing the bottle. The opposite is also true; giving too many bottles can result in breast refusal.
What can I do if my baby refuses the bottle?
This is a tricky situation requiring much patience; but here are some tips to help.
- Some babies will refuse the bottle if mom is around. Let dad or another caregiver try while mom steps away.
- Since the baby associates feedings with the mother, she may be the only one who can successfully offer the bottle at first. Once started, switching mid-feed might be possible.
- Try different positions and places. Try with the baby in a breastfeeding position, or turned outward with baby’s back on parent’s chest, bounce on the yoga ball, in the bouncy seat, or in the stroller.
- Try distraction. Walk around looking at different things. Go outside. Offer a pacifier and then switch to the bottle. Offer the breast and then switch to the bottle. Try with baby under a mobile. Let the baby play with the bottle when it’s not feeding time. Warm the bottle nipple or dip it in warm milk before starting.
- Use fresh, not frozen milk. Try it both warm and cold.
- Keep it a happy time. Try once or twice a day for a few minutes when everyone is relaxed. Think of it as a practice time. Try at a time when the baby is only a little bit hungry. If the baby begins to cry—stop and try again later. Wait 10 minutes before nursing.
Important reminders
- Remember to keep a positive attitude and do not allow bottle feeding to result in a frustrated baby and tearful parents.
- Don’t let the partner always be the bad guy. Find other nurturing people to help.
- Don’t withhold food for long periods. It’s a myth that a super hungry baby will more likely take the bottle. Babies need time to learn this new skill; they are not just being stubborn.
- A successful bottle feed might just be a small quantity at first. Celebrate even the small steps.
What is engorgement and what are tips for relief?
Medical Dictionaries define engorgement as congestion or distention with fluid.
In breastfeeding, engorgement actually refers to the time just after birth (between days 2 and 5) when the milk supply is said to be “coming in”. It is caused by increasing milk supply, increased circulation to the breast, and retained fluid in the tissues. This increased fullness in the breast is actually a positive sign showing that these breasts are working well, milk supply is increasing, and things are progressing as they should. It usually resolves in 24-48 hours if the baby is nursing well. But in some mother’s, engorgement can become severe, resulting in hard, hot, red, swollen breasts which can make it difficult for the baby to latch deeply and nurse well. Left unchecked, severe engorgement will cause a rapid lowering of the milk supply. But it is usually preventable. Frequent and effective milk removal right from the start is the key. If a baby is nursing well, no treatment should be necessary at all.
Here are some tips to prevent and treat severe engorgement.
- Latch deeply. Take a prenatal breastfeeding class with your partner to learn how.
- Get help. Lactation consultants can help in the hospital, at home, and virtually. Check out online videos as well.
- Nurse right away, within the first two hours after birth.
- Nurse very frequently. Feed as often as the baby wants to, but at least every 2-3 hours around the clock.
- If the baby is unable to latch and is unable to nurse well, pump with an excellent pump at least every 2-3 hours—8+ times in 24 hours.
- Hot compresses or a hot shower before the feed can help with milk flow, and cold compresses after the feed can reduce inflammation.
- Breast massage before and breast compressions during the feed can be helpful.
- Anti-inflammatory medication like Ibuprofen or Motrin are often ordered by the physician for post-birth discomfort and can be helpful to also reduce breast inflammation.
There are other times when a mom describes her breasts as engorged. This can be when the breastfeed was delayed or skipped as when the baby sleeps longer than expected. Quickly going back to frequent emptying of the breast should solve the feeling. Remember, the more often a breast is emptied, the better the milk supply. The poorly, or infrequently emptied breast results in a lowered supply.
Will eating peanuts while breastfeeding help food allergies?
No, there is insufficient evidence showing that consuming allergenic foods while breastfeeding can help. This was supported by the the 2019 Guidelines from the American Academy of Pediatrics (AAP) announcing that “no conclusions can be made about the role of breastfeeding in delaying the onset of specific food allergies.” Therefore, I recommend early and sustained allergen introduction, regardless of a mother’s diet while pregnant and/or breastfeeding.
At The Pump Station & Nurtury, we recommend Ready. Set. Food! because it lets mothers continue exclusive breastfeeding while also starting early, sustained allergen introduction. Ready. Set. Food! easily dissolves in breast milk, so breastfeeding mothers can continue to exclusively nurse without having to introduce solids before their baby is ready.
About Corky Harvey, MS, RN, IBCLC: Corky is the founder of The Pump Station & Nurtury, the first new parent resource center of its kind. She is a registered nurse with a Master’s degree in maternal/newborn nursing from the University of Maryland. She is an International Board Certified Lactation Consultant, a certified Happiest Baby on the Block educator, and was a long-time Childbirth Educator. Corky does one-on-one lactation consultations, teaches Prenatal Breastfeeding, Baby Care, and new Grandparents classes. She was on the faculty of the UCLA Lactation Educator and Consultant programs for many years and still lectures at hospitals, conferences and parent venues. Corky has three grown children who were breastfed and she loves to claim that their intelligence is linked to this. In her spare time she enjoys traveling with her husband Dean, especially to Germany where her two darling grandsons live.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
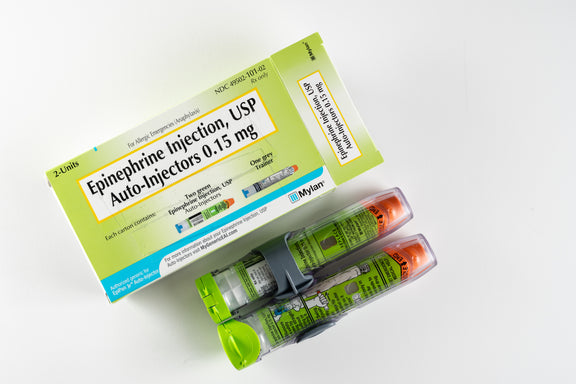
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.

