Research has revealed that Asian, Black, and Hispanic individuals, and individuals in lower-income families, are more likely to shoulder the burden of food allergies. Learn about what this vital study’s findings mean for families.
Recent research published in the Journal of the American Medical Association (JAMA) has revealed that Asian, Black, and Hispanic individuals are more likely to have food allergies than their White (non-Hispanic) peers, and individuals in lower-income families are more likely to have food allergies than individuals in higher-income families. Today, we’ll give an overview of this vital study’s findings, plus what they mean for families.
Why is this study so important?
Food allergies affect around 1 in 13 children and 1 in 10 adults in the U.S. And when someone has a food allergy, they experience many health, economic, and social burdens.
Eating even a small amount of their allergen will cause their body to develop an allergic reaction, and any reaction could become severe or even life-threatening.
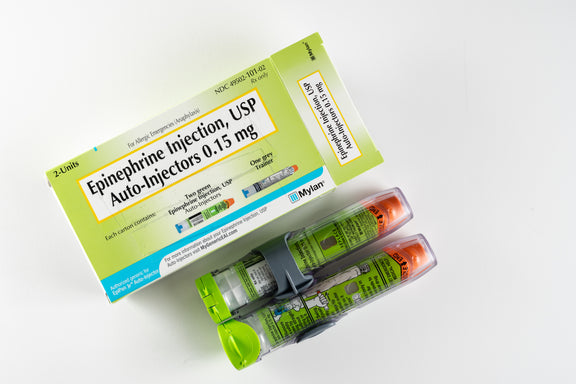
As a result, people with food allergies must buy and carry epinephrine in case of a severe allergic reaction, and they may need to visit the emergency room if a reaction turns severe. They might also need to buy more expensive foods in order to avoid foods that contain their allergen(s).
But who is most likely to carry the burdens of food allergies?
Before this study, there was research available about the differences in food allergy rates between Black and White populations. But there wasn’t much information available about food allergy rates among other racial and ethnic groups, and there wasn’t much information about food allergy rates in different socioeconomic groups. This study aimed to change that.
What did the study involve?
In 2015 and 2016, researchers ran a cross-section survey online and via telephone, to examine food allergy rates across different groups. They made sure the demographics of people surveyed accurately reflect the racial, ethnic, and economic diversity in the U.S. population.
- The survey was administered to 78,851 individuals in the U.S., in 51,819 households.
- 40,443 of these people were adults who answered the questions themselves
- 38,408 were children whose parents or caregivers answered the questions for them.
- The survey asked if anyone in the household had a food allergy to one or more of the top 9 allergens (cow’s milk, egg, peanut, tree nuts, soy, wheat, sesame, finned fish, and/or shellfish), and if so, which one(s).
- This survey also asked for data about each individual's race, ethnicity, and household income.
- To be counted as having a food allergy, someone either needed to:
- Have an allergy diagnosed by a doctor, or
- Have symptoms that convincingly pointed to a food allergy (and not to a food intolerance or other illness)
- The survey also asked people with food allergies about their experiences, including:
- Whether they've had at least one severe allergic reaction
- Whether they've used an EpiPen before
- Whether they've visited the emergency department because of a food allergy
- The results of this survey were analyzed in 2022 and 2023.
Key results of the study
The study's results found that:
- Black, Hispanic, and Asian individuals were more likely to have a food allergy than White individuals
- People in lower-income families were more likely to have a food allergy than their higher-income peers.
- Non-White and lower-income families were also more likely to shoulder significant burdens of food allergy, like dealing with a severe reaction or visiting the emergency department.
- And Black individuals are most likely to have multiple food allergies.
Breaking down the findings
Food allergy rates across racial and ethnic groups
- Across all age groups, 10.6% of Black individuals, 10.6% of Hispanic individuals, and 10.5% of Asian individuals had at least one food allergy. Meanwhile, 9.5% of White individuals had at least one food allergy.
Food allergy rates by socioeconomic status
- Food allergy rates were highest in households earning $50,000-$99,999 per year.
- Food allergy rates were lowest in households earning $150,000 or more per year.
- Individuals in households earning less than $100,000 per year were more likely to have a food allergy than individuals in households earning $100,000 or greater.
Types of food allergies in children
- Black children were more likely to have a peanut allergy or egg allergy than their peers of other races and ethnicities.
- Asian children were more likely to have a tree nut allergy than their peers of other races and ethnicities.
Multiple food allergies
- Black individuals were most likely to have more than one food allergy.
- 50.6% of Black individuals with food allergies reported allergies to more than one food.
Severe allergic reactions
- Black and Hispanic individuals had severe allergic reactions (food allergies that caused severe symptoms in more than one organ system) most often.
- 55.8% of Black individuals with a food allergy had at least one severe allergic reaction.
- 51.3% of Hispanic individuals with a food allergy had at least one severe allergic reaction.
EpiPen access and use
- Hispanic and Black individuals are most likely to have used an EpiPen to stop an allergic reaction.
- 24.6% of Hispanic individuals with food allergies, and 23.6% of Black individuals with food allergies, have used an EpiPen at least once.
- More Asian individuals have also used an EpiPen than their White peers.
- 22.6% of Asian individuals with food allergies have used an EpiPen at least once, compared to 20.9% of White individuals with food allergies.
- Individuals with food allergies whose household earned less than $50,000 per year were the least likely to have an EpiPen prescription.
Emergency department visits
- Hispanic and Black individuals were most likely to visit the emergency department in the last year because of a food allergy.
- 15.5% of Hispanic individuals, and 13.5% of Black individuals, needed food allergy emergency care within the year.
- Hispanic and Black individuals were also most likely to visit the emergency department at least once over their lifetime because of a food allergy.
- 47.7% of Hispanic individuals, and 45.4% of Black individuals, needed food allergy emergency care at least once over their lifetime.
- Individuals in households earning less than $25,000 per year were most likely to need emergency care for a food allergy (both over the past year and in their lifetime).
What do these findings mean for families and the community?
Non-White individuals, and families with lower household incomes, are more likely to shoulder the burdens of food allergies than their White and higher-income peers.
This means it’s especially important to improve allergy care access for communities of color and lower-income communities. Pediatricians and insurers should make sure lower-income families can access and afford allergist care and epinephrine prescriptions. After all, previous research has shown that allergist care can lower food allergy treatment costs for peanut-allergic children and their families.
It’s also vital to make foods free of the top 9 allergens available at a low cost, to reduce the likelihood of allergic reactions in lower-income communities (and thus reduce the likelihood of severe reactions and emergency room visits).
Another important step to address the disproportionate food allergy burden is raising awareness of early allergen introduction, particularly among non-White and lower-income families. After all, studies have shown that introducing common allergens to babies early and often gives them the best chance at a future of food freedom, where they’re able to eat these common allergen foods without fear of an allergic reaction.
Ready. Set. Food! is committed to making food freedom accessible to all babies, including those whose families need financial assistance. Through our Giving Back program, Ready. Set. Food! has distributed free 6-month plans of our early allergen introduction system (Stages 1 and 2) to low-income families.
Many of our Giving Back program families have applied for assistance online. But through Memorial Hermann Health System, we’ve educated low-income families on early allergen introduction in person along with distributing free 6-month Ready. Set. Food! plans. At the 4-month-old well-child visit, along with talking to parents about vital early allergen introduction guidelines, pediatricians give the Ready. Set. Food! allergen introduction system to families in need of assistance.
-------------------------------
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease.
See the FDA Peanut Allergy Qualified Health Claim at the bottom of our homepage.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.
