Oral allergy syndrome is also called Pollen Food Allergy Syndrome. Learn what oral allergy syndrome is, common symptoms, and how to manage and treat it
Does your child suffer from an itchy mouth when eating certain raw fruits or vegetables? They may be experiencing oral allergy syndrome. Today, we’ll break down what oral allergy syndrome is, common symptoms, how oral allergy syndrome is diagnosed, and tips for managing oral allergy syndrome.
What is oral allergy syndrome?
Oral allergy syndrome (OAS) is also known as Pollen Food Allergy Syndrome (PFAS). It’s an allergy to certain raw fruits and vegetables (and sometimes, raw tree nuts). It only appears in children and adults who already have pollen allergies.
People with pollen allergies already develop immune system responses, like congestion and coughing, when their bodies are exposed to certain kinds of pollen.
When someone with a pollen allergy develops oral allergy syndrome, their immune system recognizes that proteins in certain types of raw fruits and vegetables are extremely similar to the structure of the pollen that they are allergic to.
Each time this person eats certain raw vegetables or fruits, their immune system thinks the fruit and vegetable proteins are the same as the “problem” pollen. So, it causes symptoms of an allergic reaction to develop, to over-defend the body against these proteins. (This is known as cross-reactivity.)
But when the “problem” fruits or vegetables are cooked, the proteins are usually changed enough that the person’s immune system doesn’t think that the proteins are the same as the “problem” pollen. This means that many people with oral allergy syndrome can eat cooked versions of their “problem” fruits and vegetables.
Learn more about oral allergy syndrome from the American Academy of Allergy, Asthma, and Immunology (AAAAI):
Who develops oral allergy syndrome?
Oral allergy syndrome is extremely rare in babies and toddlers under the age of 3. This is because children don’t usually develop hay fever (a common reaction from allergies to pollen) until after the age of 3. And someone who develops oral allergy syndrome will always have pollen allergies first.
Oral allergy syndrome is more common in older children, teens and adults. Sometimes, a person will eat certain fruits or vegetables for years before they become “problem” foods.
Anyone with a pollen allergy could develop OAS. But according to the American College of Allergy, Asthma and Immunology (ACAAI), people with birch, ragweed or grass pollen allergies are most likely to develop OAS.
How oral allergy syndrome is diagnosed
To diagnose oral allergy syndrome, an allergist will take a look at your child’s health history, especially their history of pollen allergies and potential reactions to food. They might also use a skin prick test or oral challenge with raw fruits or vegetables.
Cross-Reactivity: Which Pollens Are Similar To Which Foods?
Here are the fruits, vegetables and tree nuts that are similar to certain pollens, and that may cause cross-reactivity (symptoms of an oral allergy syndrome reaction) when someone has OAS. Our list is based on information from the ACAAI and the Children’s Hospital of Philadelphia (CHOP).

Oral allergy syndrome symptoms
In the vast majority of cases, oral allergy syndrome symptoms only appear in the mouth and on the face area. They usually occur within minutes of eating a “problem” food, and usually stop quickly when the “problem food” is spit out or swallowed.
The most common symptoms of OAS include:
- Itchy or tingly mouth
- Itchy or tingly tongue
- Scratchy throat
- Sneezing
- Congestion
- Swelling of the lips, mouth, tongue, or throat
- Hives on the mouth area (sometimes)
- Itchy ears (sometimes)
OAS reactions are usually mild, and rarely ever severe. They are usually milder than traditional food allergy reactions.
However, a very small percentage of people have developed a severe reaction, and an even smaller percentage have developed anaphylaxis (a whole-body, life-threatening allergic reaction) from OAS.
The ACAAI reports, “In one study, researchers found that PFAS,” also known as oral allergy syndrome, “progressed to systemic symptoms in nearly 9 percent of patients [of all ages] and to anaphylactic shock in 1.7 percent of patients [of all ages].”
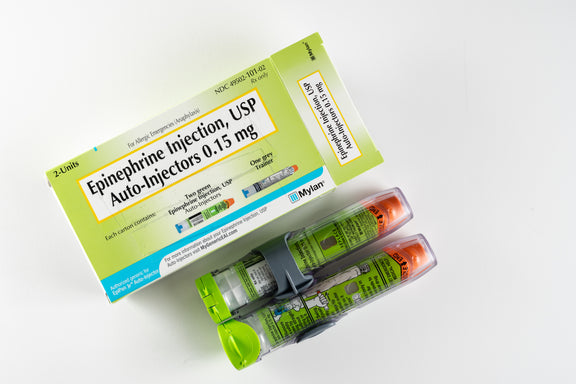
If oral allergy syndrome causes any symptoms beyond the mouth and face area, the food that caused the reaction could be an anaphylaxis risk. Your allergist will determine if your child should carry an EpiPen (the only way to reverse severe allergic reactions) in case of a potential severe OAS reaction.
Managing and treating oral allergy syndrome
The number one way to manage oral allergy syndrome is making sure your child avoids eating raw forms of the foods that cause an OAS reaction.
Sometimes, peeling a fruit or vegetable can reduce the likelihood of an OAS reaction, since the protein that causes the OAS reaction is often on the fruit’s or vegetable’s skin. This doesn’t always work, though.
And often, cooking or heating your child’s problem foods will be enough to change the protein structures, so your child will be able to eat them with no issue. But if your child still experiences symptoms after foods are cooked or peeled, they’ll need to avoid those foods completely.
Since oral allergy syndrome reactions usually stop quickly when the “problem food” is spit out or swallowed, treatment often isn’t needed. There are treatments available, though.
During an OAS reaction, giving an antihistamine (like Zyrtec) may help relieve mild symptoms. But if your child is under the age of 6, be sure to ask an allergist.
For more severe cases that appear often, allergy immunotherapy shots for the pollen someone is allergic to may be helpful in treating OAS. But this treatment type has had mixed results. Sometimes, the shots help people become more tolerant of “problem foods,” but don’t completely stop OAS symptoms.
And as the ACAAI advises, if your child experiences “significant throat discomfort or difficulty swallowing,” has “systemic symptoms” (symptoms that affect areas of the body other than the face), has “reactions to cooked forms of the foods,” or has OAS “symptoms to high-risk foods” like tree nuts, talk to your allergist. They may prescribe EpiPen auto-injectors in case of a more severe allergic reaction.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.

