In honor of Food Allergy Action Month, we're excited to kick off our Ask the Allergist series, focused on providing food allergy education to families. At Ready. Set. Food!, we’re committed to all aspects of food allergy education, so families can make informed decisions about their children’s nutrition.
What Is A Food Allergy?
A food allergy occurs when the body’s immune system mistakenly responds to certain foods that it thinks are harmful. Our immune systems defend and protect us from foreign invaders like certain viruses and bacteria.
Food allergies occur when the immune system over-defends and treats certain proteins in foods as foreign invaders. These proteins are called allergens and our immune systems make special allergy antibodies called IgE antibodies to these allergens to help fight them off. These antibodies can help our cells cause a reaction each time a person eats a food they are allergic to.

When the symptoms are severe and involving more than one organ system it’s classified as anaphylaxis, and this can be life threatening.
In babies, hives and vomiting are the most common symptoms of a food allergic reaction. These symptoms usually occur within seconds to minutes and almost always within 2 hours. In addition, one reaction can vary widely from the next in the same person. One cannot predict what type of reaction a person will have each time they eat a food that they are allergic to. Food allergies are most common in children, but a food allergy can occur at any age.
IgE-mediated v. Non-IgE-mediated food allergy
- IgE-mediated food allergy is different than non-IgE-mediated (delayed-type) food allergy
- For instance, some infants have a delayed allergy to milk which can cause blood and mucus in the stool hours to days after the ingestion of milk.
- Another example is Food protein-induced enterocolitis syndrome (FPIES) which is a non-IgE-mediated disorder that usually occurs in young infants. Symptoms include chronic vomiting, diarrhea, and failure to gain weight or height. When the allergenic food is removed from the infant’s diet, symptoms disappear. Milk and soy protein are the most common causes
Food Allergy Testing
Validated food allergy tests like skin prick tests or blood tests look for the presence of IgE antibody. If the tests are positive, they show that a person produces IgE antibodies to food allergens. But blood and skin tests alone cannot be used to diagnose food allergy. A person does not have a food allergy unless they also have clinical symptoms. There is also a chance that a person could have a "false positive" on their skin or blood test.
An oral food challenge which exposes a person to their potential allergenic food in small doses, slowly increasing over time with careful observation in a medical facility to watch for signs of an allergic reaction, is the only way to definitively diagnose a food allergy.
While an oral food challenge is the only way to definitively diagnose a food allergy, they can also be risky.
However oral food challenges can be risky, thus many times they are avoided and a diagnosis is made based on the other tests above plus the person’s medical history. A patient’s medical history (their reported experiences after exposure to the specific food) is the most important part of the evaluation for a food allergy diagnosis.
A Recent Breakthrough in Food Allergen Introduction
Thankfully, recent landmark studies (LEAP, EAT, PETIT) have proven the importance of early allergen introduction. In addition, new medical guidelines from the American Academy of Pediatrics, the National Institutes of Health (NIH), and the American Academy of Allergy, Asthma, and Immunology (AAAAI) have been published supporting early and sustained allergen introduction.
Along with a team of leading allergy experts and parents, I helped develop Ready. Set. Food!, a gentle, guided system based on these medical guidelines. After over a year of research and development, we're proud to offer Ready. Set. Food! to families like yours, making it as easy and safe as possible to introduce babies to peanut, egg, and milk in the amounts used in the landmark clinical studies.
About the author: Our Chief Allergist, Katie Marks-Cogan, M.D., is board certified in Allergy/Immunology and Internal Medicine, and treats both pediatric and adult patients. Originally from Cleveland, Ohio, she received her M.D. with honors from the University of Maryland School of Medicine. She then completed her residency in Internal Medicine at Northwestern and fellowship in Allergy/Immunology at the prestigious University of Pennsylvania and CHOP. After finishing training, she moved to Southern California and currently works in private practice. She is a member of the scientific advisory board for Ready. Set. Food! She currently resides in Los Angeles with her husband, 4-year-old son, and 1-year-old daughter where she enjoys hiking, building LEGO castles with her kids, and cooking with her family.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
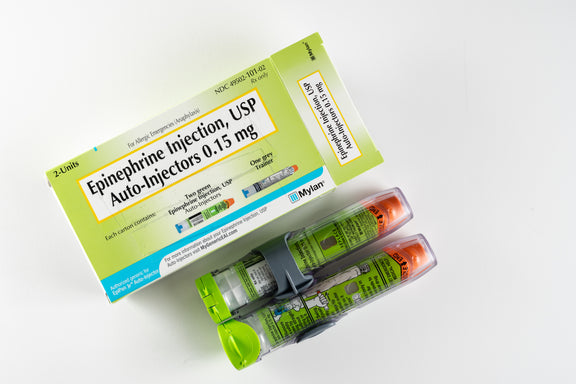
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.

