If your baby experiences vomiting, diarrhea, and fussiness, they may be diagnosed with cow’s milk allergy. But is your baby really allergic to cow’s milk?
When their babies are diagnosed with cow’s milk allergy, breastfeeding moms have to cut out cow’s milk from their diet. Since many foods contain cow’s milk, this can be a struggle. Meanwhile, parents of formula-fed babies have to switch to a specialized formula. This formula can be expensive but also the only option for many families.
But a recent study published in JAMA Pediatrics shows that milk allergy is over-diagnosed: many babies who are diagnosed with a milk allergy don’t actually have one.
According to this study, while 14% of families think their baby has a milk allergy, only 1% of babies actually have a milk allergy.
In this article, we’ll:
- Examine the two types of cow’s milk allergies, including how one type is harder to diagnose
- Break down the findings from the JAMA study
- Explain what the findings mean for families, including for introducing milk to your baby
Two Types of Milk Allergies: IgE v. Non-IgE Mediated
There are two types of cow’s milk allergy or cow’s milk protein allergy (CMPA). Both involve the immune system. Also, vomiting is a common symptom of both. However, there are many differences between the two types, and one is much harder to confirm than the other.
The first type is known as IgE-mediated milk allergy.
- People with this type of milk allergy produce IgE antibodies that over-defend their body against cow’s milk, and cause an allergic reaction.
- This type of milk allergy usually causes more typical food allergy symptoms, such as hives and swelling.
- Symptoms of an IgE-mediated milk allergy show up seconds to minutes after baby consumes milk, and almost always occur within two hours.
- These symptoms combined with proper testing make IgE-mediated milk allergy easier to diagnose.
The second type is known as non-IgE-mediated milk allergy, or delayed-type cow’s milk allergy.
- This type of allergy commonly causes symptoms like bloody stools, fussiness, and diarrhea.
- It is harder to diagnose, because babies might have symptoms like these for reasons other than cow’s milk allergy.
- The most common type of non-IgE-mediated allergen is cow’s milk. FPIES (Food Protein-Induced Enterocolitis Syndrome) is also a type of non-IgE-mediated food allergy with symptoms including vomiting and diarrhea.
- In addition, symptoms of this type of milk allergy tend to occur hours to days after baby consumes milk.
- Many babies are misdiagnosed with this particular type of allergy.
- The only way to figure out if your baby has this type of allergy is to remove milk from your baby’s diet (as well as your own if you're breastfeeding).
- Then, see if their symptoms improve once you've removed the cow's milk.
- After this, reintroduce milk and see if these symptoms appear again.
- Even if the symptoms seem tied to milk, though, they could stem from a milk intolerance and not a milk allergy.
The JAMA study: Key Takeaways
The JAMA study reviewed nine sets of guidelines related to cow’s milk allergies in babies, published from 2012 to 2019, against clinical research on cow’s milk allergies. In particular, it examined the rates of confirmed vs. diagnosed cow’s milk allergies in babies.
According to this study:
- 14% of babies are diagnosed with milk allergy, but only 1% have a confirmed milk allergy.
- Some doctors may be too quick to associate common baby symptoms, like rashes, vomiting, and fussiness, with milk allergy.
- This may lead parents to believe their baby has a milk allergy when they don’t actually have one.
- “Clinical trials do not provide consistent support” for removing cow’s milk from a baby’s diet “to manage common symptoms in infants without proven cow’s milk allergies.” In other words, elimination diets and specialized formula may be unnecessary for many babies.
- Also, even if their baby has a confirmed cow’s milk allergy, breastfeeding mothers don’t need to avoid cow’s milk.
- In over 99% of babies with proven cow’s milk allergies, their mothers’ breastmilk didn't contain enough cow’s milk protein to trigger an allergic reaction.
- The authors of 81% of the cow’s milk allergy guidelines said they had a conflict of interest with formula manufacturers.
- Also, three of the reviewed sets of guidelines were directly supported by formula manufacturers.
- So, there is growing criticism over the potential bias of these guidelines.
What do the findings mean for families?
- Many parents are told that their child has a milk allergy when they don’t actually have one.
- This causes parents to eliminate cow’s milk from their baby’s diet when they don’t have to.
- If your doctor says that your baby may have a cow’s milk allergy, remember that a food challenge is the only way to know for sure.
- Blood testing and skin prick testing may help you find out if your baby has a milk allergy, but these tests aren’t always reliable.
- Talk to your doctor to understand why they gave your baby the diagnosis, and ask if it makes sense to perform any tests to be sure baby has an actual allergy. Ideally, work to get a clearer picture before making dietary changes.
- Removing cow’s milk from your baby’s diet is not recommended unless your baby has a confirmed milk allergy.
- In fact, if your baby doesn’t have a milk allergy, feeding them cow’s milk products early and often is important.
- If you’ve already removed milk from your or your baby’s diet, and your baby doesn’t have a confirmed milk allergy, talk to your doctor about reintroducing milk to your baby.
- Remember that irritability, digestive problems, and abnormal stools are common symptoms in babies that often improve on their own after several months.
- An allergy isn’t always the cause of these symptoms.
Milk allergy vs. Milk intolerance
Milk protein intolerance could be another possible cause of your baby’s digestive symptoms, including bloody stools and irritability.
Milk intolerance isn’t the same as milk allergy, because it doesn’t involve the immune system. But milk intolerance and milk allergy are often confused, since both are sensitivities to milk protein, and both share similar symptoms. (Learn more about milk intolerance here.)
Doctors typically recommend reintroducing milk to babies with a delayed allergy to milk or milk intolerance at some point. So, if you’ve already removed cow’s milk from your or your baby’s diet, talk to your pediatrician or allergist about when to reintroduce it.
Landmark clinical studies have shown that introducing babies to cow’s milk early and often can help. Find out more about early introduction of cow’s milk, as well as peanut and egg, here.

Pros And Cons Of Sippy Cups
Thinking about giving your little one a sippy cup? Today, we’ll co...

What Toddlers Eat In A Day: 12-18 Months Old
Looking for ideas of what to feed your 12-18 month old little one? ...
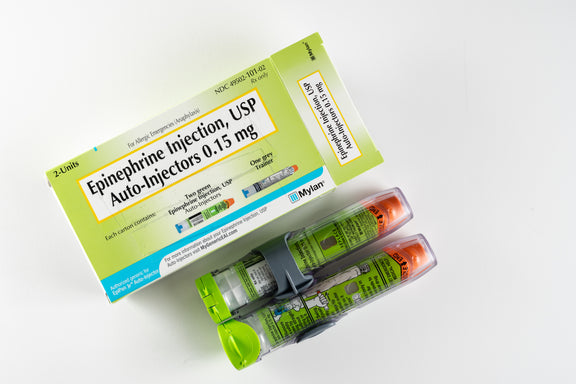
New Study Shows That Infant Anaphylaxis Usually Resolves With One Epinephrine Dose
A recent study has shown that, when infants experience severe aller...

Pregnancy Nutrition: What To Eat In The First Trimester
What to eat in the first trimester that will nourish your body, pro...

Formula Feeding Amounts: How Much Formula Should You Feed Baby Per Day?
How much formula should baby drink per day? It depends on their age...

What Baby Eats In A Day: 6-12 Months Old
Looking for ideas of what to feed your 6-12 month old little one? H...
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease. If your infant has severe eczema, check with your infant’s healthcare provider before feeding foods containing ground peanuts.

